I missed the phone call. The voicemail made my heart drop. The NICU nurse called to say my baby was stable, but I needed to call back. Thankfully we only got this call once during his 39-day NICU stay. Once was more than enough.
Continue reading “When Your Baby Aspirates”St. Patrick’s Day NICU Graduation
Growing up I looked forward to St. Patrick’s Day. My brothers and I would make elaborate leprechaun traps and imagine what it would be like to catch one. We would wake up to gold coins and fool’s gold and other treats and goodies scattered around our bedroom. But St. Patrick’s Day has a whole new significance for me now.
Continue reading “St. Patrick’s Day NICU Graduation”Our G-Tube Journey
This post contains affiliate links. I get commissions for purchases made through these links.
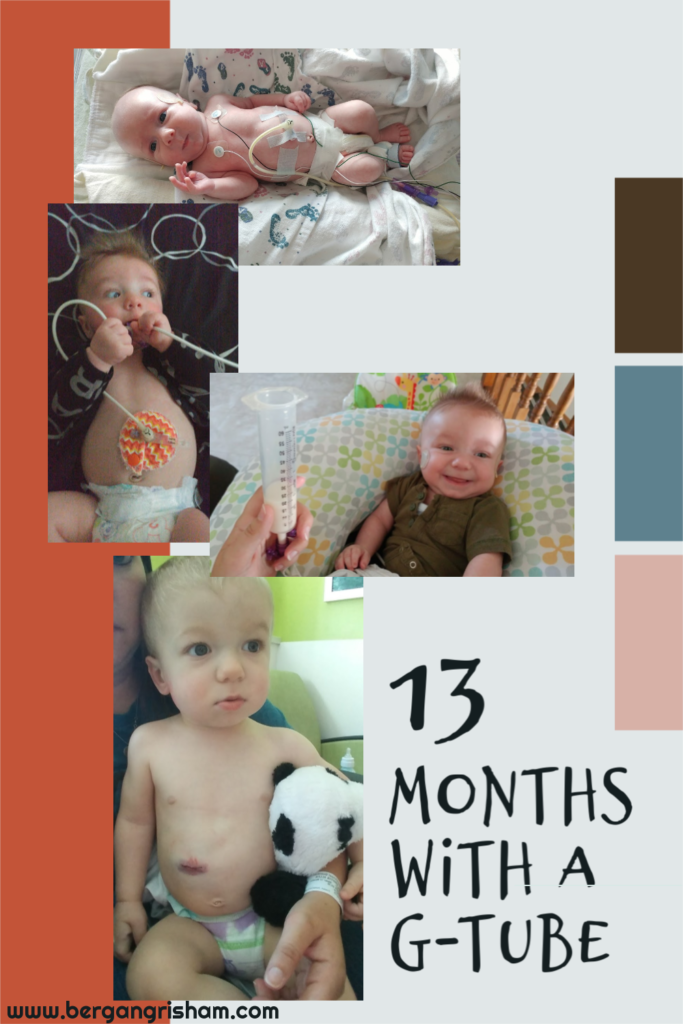
This last week was Feeding Tube Awareness Week. Even though a year ago I felt pretty confident in my feeding tube knowledge and experience, I felt a little strange about it this year. My little guy had a g-tube for all of 13 months. He was only fed fortified breast milk and formula through his tube. I know of so many families who use feeding tubes for years and years. But I decided that every feeding tube story is important, so here is ours:
My little man got his g-tube at five weeks old. He’d had problem after problem and after aspirating, being diagnosed with reflux and larygnomalacia, being NG-tube fed for weeks, taking medications, and trying thickened milk, he aspirated again. The doctors called us in to have a chat. Because my husband and I both wanted to be there and we had our two-year-old, we met in a conference room outside of the NICU.
Basically, they simply recommended a g-tube. I’d guessed as much and jumped right on board. I had no idea what I was getting into, but after nearly 5 weeks of trying to find solutions, I would have done anything to get my little boy home. It took a few days to get him transferred to the children’s hospital that could place the tube and several more days to get the ball rolling.
I got to the hospital early on surgery day. I snuggled my little guy and waited while the surgery time moved later and later. I finally took him down with the nurse and watched the doctor wheel him away. Conveniently enough, the g-tube class was taught right during his surgery. My parents and husband came and took the class with me so several of us would know how to take care of him. To be honest, I got pretty lightheaded as the teacher explained everything. I started to question whether I could handle the tube.

Griffin had never had to be intubated, so that was hard to see. I was scared to hold him with the tube. I didn’t want to hurt him or accidentally pull it out. Over the next several days I learned about caring for the tube site and feeding him through the tube. To be honest, I didn’t feel very prepared when we took him home five days post-op, but I learned quickly. I had to. We had home health visits for a few weeks and lots of check-ups. I asked every question, even the ones that seemed silly. I didn’t want to do anything wrong.
Medical supplies soon became our new normal. From the feeding pump and pole to the piles of tape and gauze and ointments to the pump parts and syringes and milk storage bottles I had to wash constantly. It started to seem weird that there were people who didn’t feed their baby with a tube…which is especially strange since my first son was simply breastfed. I guess you just get used to whatever your current normal is.

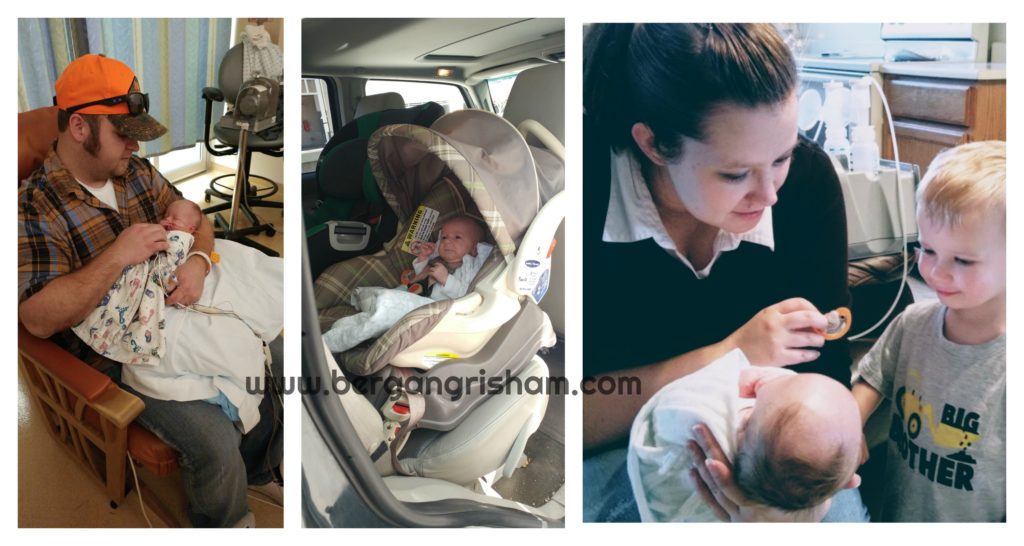
My older son was 2.5 and didn’t have really any experience with babies, and especially not with how they are fed. Griffin’s 39-day stay in the NICU was his normal. Griffin’s feeding tube was his normal. We taught him to be careful with the tube. The hospital gave him a little doll that had a g-tube and a bunch of supplies, so he got to practice taking care of his baby. It amazes me how kids can adapt. I had been so worried about splitting my time and taking care of two littles. Turns out, all the medical stuff took even more time than I expected taking care of another child would take. And yet my toddler handled it so well.
Because Griffin aspirated, he got all of his nutrition through his tube. This meant that I couldn’t breastfeed. In the beginning of our NICU stay, the plan had been to work on breastfeeding, but after he aspirated twice (the second time on thickened milk), all hope of breastfeeding went out the window. Because I had already been pumping for weeks and felt like it was one of the only things I could do for him, I kept going. It was time consuming, but I didn’t mind it too much.
It got harder when Griffin came home from the hospital. I pumped for over three months before my toddler started to be obviously upset by it. He didn’t like how much time I spent attached to the pump. Because of all he was going through with this and for my own sanity in the situation, I slowly stopped pumping for him. I had so much milk saved in the freezer that I was able to give Griffin fortified breast milk for the first six months, and I don’t regret stopping at all. It was what was best for us.

I slowly learned how to balance everything. I stopped using the pole for the feeding pump during the day and just left the feeding pump in the backpack. That gave us more freedom to move around the house and made us more prepared to leave the house. I just made sure to plug the pump in when Griffin was sleeping so it wouldn’t die. He was on a schedule of being fed over an hour starting every three hours and then nine hours at night. As a result, our longest time without the pump was two hours.
It is hard to leave the house and get back in two hours, especially with two little kids. So we learned to feed on the go. I started babywearing once his tube site was healed enough. My Tula Free-to-Grow carrier was the best for this. The strap was perfect for clipping the backpack onto with a carabiner.

Life felt pretty crazy for a while. But crazy in a good way. I allowed myself some grace because I knew there would be an adjustment to two kids, plus there were so many appointments and therapies and dozens of other things I hadn’t expected. I have several pictures like the following one from that time. When I’d look around the room or the house and realize just how much chaos there was. This picture was from when we still used the pole for the feeding pump. You can see Mr. Griffin on his play mat and my breast pump next to him. I had to multitask feeding him, entertaining him, pumping more milk, entertaining my toddler, and trying to maintain my sanity.
Originally this picture made me feel a little like I was failing. Now I feel like it’s kind of beautiful.

Griffin’s feeding tube didn’t rule our lives, but it was ever present during those first six months or so. I didn’t try to hide it in pictures because that was our life. I think it shows how tough he is. We didn’t have exact expectations for how he would progress. He had hypertonia (tight muscles) and his stridor (noisy breathing) got really bad. When he was four months old he had several episodes in one week when he would turn blue/grey and stop breathing. He had surgery within the week.
Griffin had a suppraglottoplasty to get rid of the extra skin in his airway to help him breathe better. This came weeks after finding out he needed oxygen while he slept. It felt like a step backward, needing oxygen, and it felt like a huge inconvenience. He only needed it when he slept, but have you ever met a four-month-old? They sleep randomly all throughout the day. After surgery, he was able to come off oxygen for good.

For the first several months after he got his g-tube, we didn’t worry about oral feeding at all. He took a binki, which was good practice for feeding, but that was about it. We slowly started feeding thickened milk 15 ml at a time (which is NOT very much). We had a feeding therapist who came to our house. I really loved all of the connections we had with doctors and therapists. I relied on them for all the information I didn’t know about how to care for my own child. I loved sharing Griffin’s accomplishments with them. They understood how hard all of the things he was doing could be.
It took a few months before Griffin took more than half of his feeds by mouth during the day. At that point we were able to gravity feed the rest (as shown below). It was a game-changer. No more pump during the day! He still took 9 hours of feeds at night, but that was easy, and honestly, he slept through the night after like the first week home thanks to a constantly full belly.

We got the go ahead to start purees around seven months. Griffin was excited, but it was stressful. Knowing he was tiny and needed fortified food and had to have things thickened and needed every bit of nutrition we could give him was stressful. There is something to be said for tube feeding and knowing just how much your child is getting. Between bottles and gravity feeds and spitting up and trying new purees, feeding just seemed to get more complicated.
Over time we got more used to it and slowly started to thin out his milk. The feeding therapist would watch and we’d monitor how long it took him to drink and how much he drank and if we needed a different size nipple on his bottle or whether the milk was too thick or too thin. I had lists of things to look for and when to be concerned. It was a balancing act.
When he was 11 months old we did a swallow study to see whether we could get him off of thickener. No such luck. He wasn’t aspirating, but he also wasn’t handling the liquid well. He had “deep penetration” and let the liquid go all the way down to his vocal cords before correcting it. (He used thickener for another eight months or so.)
He’d barely been using his tube by that point, but because it was cold and flu season, we left it in until April, when he was 14 months old. I was so excited for them to take it out, but I was also anxious. I had been comforted by the thought that if he did get sick or wasn’t taking in enough liquid or calories, I could give more to him. It felt strange that I wouldn’t have that option.
I think I expected more from that last appointment. After all of the stressing about not letting the g-tube button come out, it was strange to just watch the doctor take the button out, cover his stoma with gauze, and send us on our way. (For the record, his button did come out twice. I was alone both times. One time he pulled it out when I was changing him. I looked from my toddler back to Griffin, and he was holding the button and examining it. The other time I was playing with him. He was on his belly and I pulled his legs to bring him back to me. Even as I was doing it I knew it was a mistake. Somehow, after the initial panic, I just dealt with it. You adapt and do what you have to do.)

I actually have a whole blog post about how Griffin healed after having his g-tube removed. Spoiler: it was not simple and didn’t go as I had planned. He ended up having his stoma surgically closed.
I am so grateful that my little man has progressed so well and no longer needs a feeding tube. But I am also so incredibly grateful that he had one. Not only did it enable us to take him home from the hospital and safely feed him, but it taught me so much. Yeah, I learned a lot about the medical side of things. But I also learned not to judge so harshly. It opened me up to a new world of families that use g-tubes. It taught me how strong I could be and how I could handle whatever I needed to for my child.
Griffin may not have a feeding tube anymore, but I still feel strongly about the importance of feeding tubes and the awareness of them.
*****I have several other posts about feeding tubes here on my blog. Check them out!*****

Griffin’s Birth Story
My little man turns 2 today! So crazy! I’ve written bits and pieces of his birth story in other posts but want to write it all out together. Griffin is my second child, and I felt more prepared going into his pregnancy and birth because I’d already done it once. I quickly learned firsthand how each birth can be very different.
Mr. Griffin was due on March 3, 2017. My first was born eight days before his due date, so I kind of guessed I’d have a February baby. I spent the whole pregnancy sure something was wrong. I worried about absolutely everything. I came up with a new worry every single day the last few weeks. My husband had to talk me through a new concern every night. I think somehow I knew something was wrong; I just didn’t know what.
Every concern I had was for naught. From thinking I was having a tubal pregnancy to thinking I had gestational diabetes and everything in between. So when I started to feel like he wasn’t moving as much that first week of February, I tried to talk myself out of worrying. I’ve always been a little confused about exact kick-count numbers but spent most of three days laying on my side, drinking cold water and juice, and counting kicks.
He always kicked “enough,” at least from what I knew. But I couldn’t shake the feeling that something was wrong. My stomach started to feel like dead weight. I hated the idea of going into the hospital “for no reason.” I didn’t want to go alone, and my husband had to work or watch our two-year-old. I finally asked my mom to go with me.
I had a bunch of monitoring done. It was so reassuring to hear his heartbeat, but I did not get good news that night. My amniotic fluid was low, and they were a little concerned about his heart rate because they couldn’t get it to accelerate like they wanted, if I remember correctly. He was practice breathing just fine. My blood pressure was okay. They sent me home with instructions to drink a ton of water to increase fluid and come back the next morning.
I went home reassured and stayed up late drinking as much water as I could. I got up the next morning, fed my toddler breakfast, dropped him off at my mom’s, and went to the hospital. Little did I know I’d be having a baby that day.
My fluid levels dropped, the baby’s heart rate wasn’t great, and my blood pressure was high. I was 36 weeks and 4 days. I sat in that room alone for what seemed like forever. I was waiting for the final decision on induction. Everyone was sure they would induce. Looking back, they probably should have induced the night before. But when they finally told me they were getting ready to move me to a delivery room for an induction, I remember the sound that came out of my mouth. It was like a wail once I was left alone again. I was so scared. I started looking up 36 weekers knowing it didn’t matter what I found online.
I texted my mom and then tried to get ahold of my husband. He was working underground in the mine near our house at the time. He didn’t have cell reception and because I wasn’t due for a few weeks, he hadn’t yet gotten the phone number I could call to get to him the fastest. It took some calling around, and he was finally on his way.
I remember sitting alone in that giant room. I had an IV in that hurt like crazy the whole day. I had my small purse and no phone charger. I had nothing I needed. I was scared for the contractions and had heard inductions are worse. With my first I got to the hospital at 9.5 cm dilated and got an epidural. This was all new to me.
I was already 3 cm dilated, which was a good sign. Contractions started slowly. My husband showed up. As the afternoon went on, things slowly went downhill. The baby’s heart rate became more concerning. They decided to put a monitor on his head but said it was very painful and recommended the epidural first. It was way different than my first. I felt so lightheaded, like I was going to pass out the whole time they placed the epidural.
My blood pressure started to go up, and when my midwife went to check me before placing the monitor, she very matter-of-factly said she could feel the umbilical cord. Everything happened so fast after that. I had no idea what that one sentence would mean for me. Everyone jumped into action putting on bootys and grabbing equipment. Somewhere in the middle of the chaos my midwife asked if I understood they were going to do a c-section. I hadn’t. I was terrified.

You see, I’m a wimp. I have a very low tolerance for pain. I’d never had surgery, and the thought of being cut open while awake was too much for me. I’d told my midwife I wanted to be asleep if I needed a c-section. When it came down to it, she convinced me to stay awake.
They put a hair cover on me and I ended up needing oxygen. I felt very faint and so scared I couldn’t think. My husband got to wear something over his clothes and come with me. I don’t know how I would have made it through that without him. They wheeled me out the door and across the hall. I had no idea we were that close to the OR.
I remember feeling so helpless staring up at the big, bright lights on the ceiling. We had to wait a little bit for the surgeon, and everyone around me was chatting and getting things ready like it was just another day for them. The anesthesiologist numbed me up to my chest and my fingers started going numb. It was so unnerving to not be able to feel or move my body. He knew I was nervous and let me know he could give me something else if I started to panic.
I’d heard that you feel tugging during c-sections. I honestly didn’t feel anything at all, thank heavens. I tried very hard not to think about what was going on past the sheet. Once Griffin was out, I was completely distracted by him. It was hard to not be able to hold him or hardly see him. They weighed him and checked him out. He was only 4 pounds but seemed fine. They wrapped him up and let my husband hold him.

I got to see his little face and get a picture of the three of us together. When they wheeled me back to the delivery room, I got to hold him. He was tiny. I tried nursing him but was scared to hold him for too long because my fingers where still a little numb and I didn’t quite trust myself.
It wasn’t long before the nurses started noticing concerns. His temperature was a little low, so they put him under the warmer. They decided to take him up the the special care nursery (they didn’t have a NICU) for a while, and I was taken to my recovery room without him. My husband spent some time with Griffin and got a good picture of him. He’d been put on oxygen by then, but you couldn’t tell how tiny he was. We hadn’t known he would be so small. 4 pounds is small, even for a 36 weeker.
We did learn that my placenta was small, which probably contributed to the IUGR (intrauterine growth restriction) and the low amniotic fluid. We had been warned that he might have some breathing issues, but he ended up with a lot more than that.
That night we let our families know what was going on. My husband went home for our bags. I was honestly thinking we’d get Griffin back to us soon. I was pretty caught up in my own recovery and have no idea how I would have cared for a newborn after the c-section. The nurses started getting me up at 3 that morning, and I nearly passed out trying to walk to and from the bathroom. It took me 24 hours to be able to stand and get into a wheelchair and not feel dizzy and lightheaded. It was 24 hours before I got to see Griffin again.
In that time they found two holes in his heart. Both of which could (and would) close on their own, but it was scary to hear.
I spent my time learning to pump, washing pump parts, resting, and trying my best not to pass out when I stood. When I was finally able to get to the special care nursery, I just sat next to Griffin holding his little hand. I wanted so badly to hold him, or at least cover him with a soft blanket. It was hard to see him so tiny, dressed in just a diaper, with monitors all over and a tube in his mouth.
The next day I got to shower and made it up to see Griffin before noon. My parents brought my toddler, Mr. Sawyer, to visit, and my mom came in to see Griffin with me. It was just the two of us when the nurse tested his blood sugar and it came back “low.” My brother has diabetes, so I know what low means. And the fact that a number didn’t even show up was not good. She seemed panicked. A guy came by a few minutes later and informed us that they couldn’t handle his care and lifeflight was on their way.

My mom went to watch Sawyer, and my dad and husband came in to give Griffin a blessing. You hear about lifeflight, but it’s not something you ever expect to need. The room was crowded with people and a huge stretcher with a glass box for my tiny baby. I watched them roll him out of the room. I watched from a wall of windows while they rolled him out to a helicopter and the helicopter flew away. My husband got to go with, my parents took Sawyer home, and thank goodness my brother showed up then. I didn’t have to be alone while I waited for news.
I guess it’s hard for me to say when the “birth story” ends because for me it is more than just the six hours of labor and the c-section. In my mind it kind of lasted until he finally came home from the hospital after 39 days. He had trouble with hypoglycemia, reflux, aspiration, laryngomalacia, stridor, and ultimately got a g-tube to be able to come home.

I have several posts about his g-tube and the NICU for those interested.
Griffin’s birth was absolutely nothing like I planned or hoped. I am so grateful for how well everything turned out. He is a happy, healthy, smart little man. He is in early intervention, but has graduated from nearly every specialty he started with. He is strong, and I feel stronger for having been through it all with him.
Happy Birthday little man!!!
What to Expect When Your Child Needs a Sleep Study

This post may contain affiliate links. I get commissions for purchases made through these links.
My little man went in for a sleep study a few weeks ago. We’re not strangers to the hospital, but this was a bit of a new experience. I wasn’t sure what to expect. The pamphlet the hospital sent me in the mail had a few tidbits of information, but I still had questions. If you are heading in for a sleep study soon, maybe you can learn a thing or two from my experience. Continue reading “What to Expect When Your Child Needs a Sleep Study”
